Did You Know?
Approximately 13 million Americans have incontinence. Of those, 85% are women.
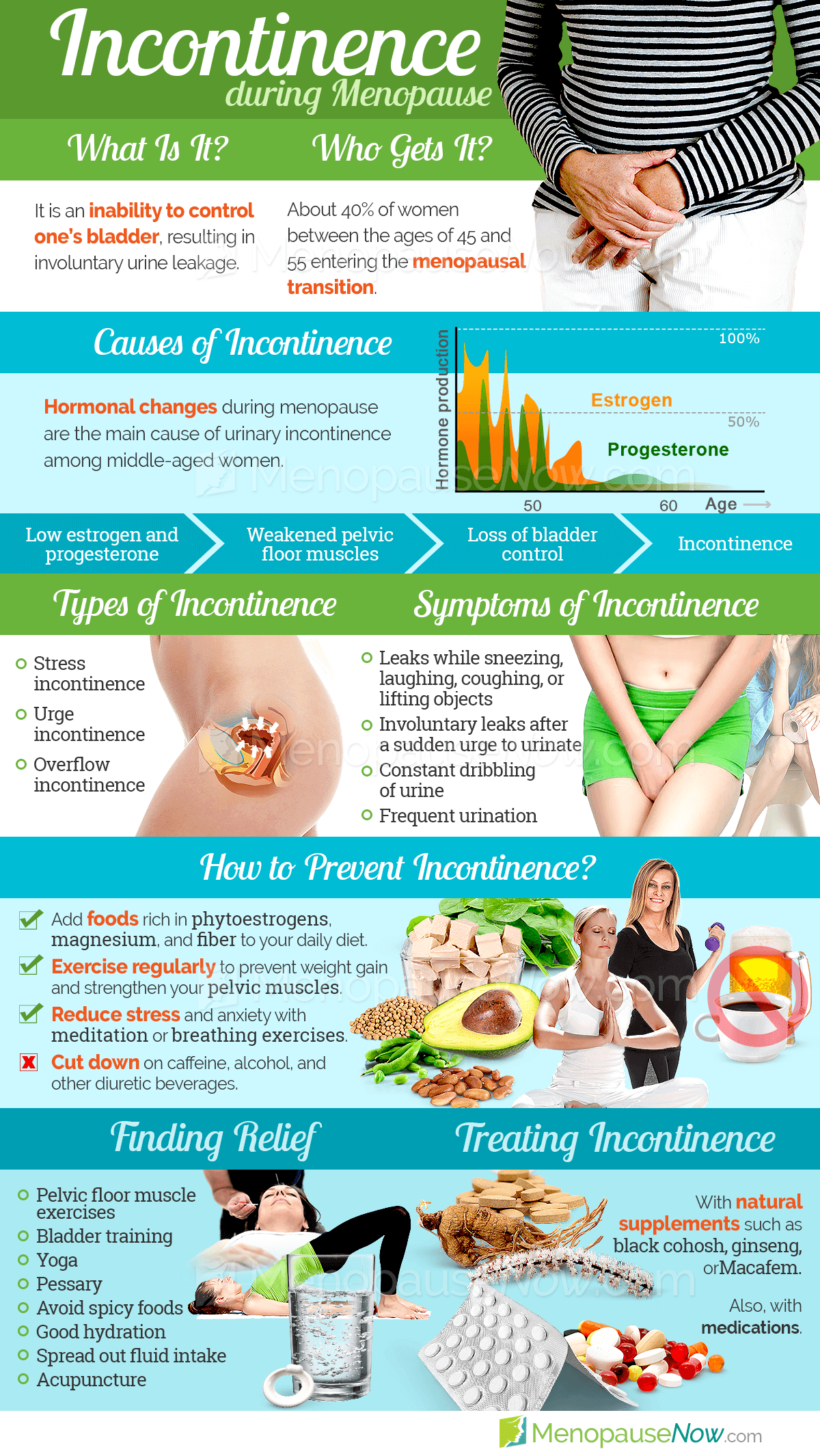
As women approach menopause, many of them experience a myriad of different symptoms, including urinary incontinence. They tend to notice the lack of bladder control, especially when sneezing, coughing, or laughing.
As a woman approaches menopause, her hormone levels fluctuate, which leads to a multitude of physical changes, including incontinence. To understand how to treat this symptom, it's best to first understand exactly what it is, what causes it, and finally, what treatment options are available. Read below to learn all about incontinence.
About Incontinence
Did You Know?
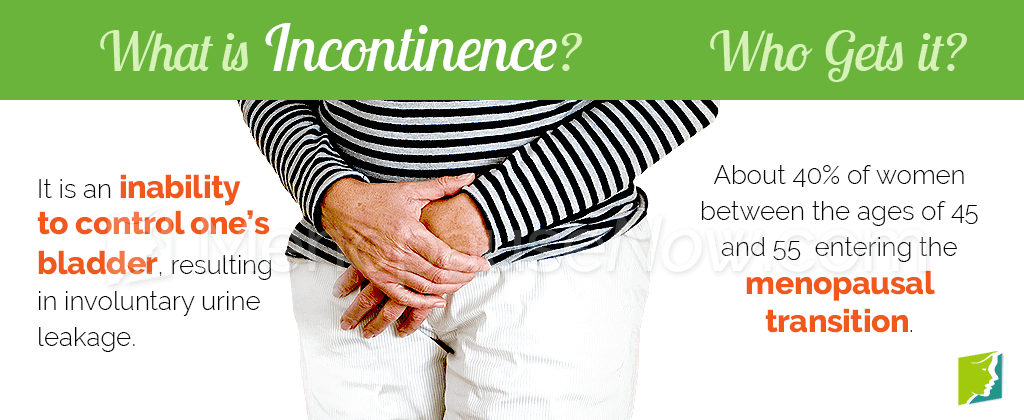
Urinary incontinence is the inability to control one's bladder. The severity can vary from woman to woman. Some women may experience occasional trickles of urine when bursting into laughter or while having a sneezing episode. Others might notice large amounts of and more frequent uncontrolled urine flows that do not seem to be stimulated by laughter or a body-shaking sneeze.
Although many women experience incontinence as they approach menopause, it is not an inevitable aspect of getting older. Fortunately, by better understanding this menopause symptom, women can treat it or prevent it from occurring. A good place to begin is with the three different types of incontinence.
Types of incontinence
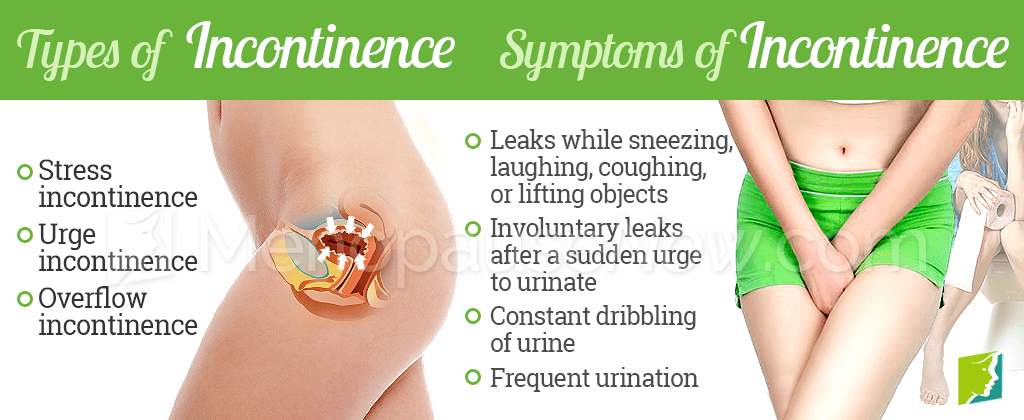
There are three main types of incontinence: stress incontinence, urge incontinence, and overflow incontinence. These types of incontinence are described in detail below.
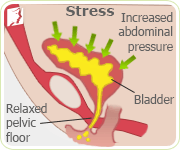
Stress incontinence is the most prominent type of incontinence women experience, especially during the menopause and postmenopause years. Women with stress incontinence involuntarily leak urine while coughing, laughing, sneezing, exercising, or lifting something. The reason these activities can cause incontinence is because they apply sudden pressure to the bladder walls, which squeezes the bladder and causes urine to leak out. This occurs as women get older is because the pelvic muscles between the bladder and the vagina often grow weaker, allowing urine to leak.
Urge incontinence is the sudden, intense, and frequent urge to urinate, immediately followed by an uncontrollable loss of urine. The bladder contracts and may give a warning of only a few seconds or a minute to make it to the restroom. Urge incontinence strikes especially while the sufferer is sleeping, drinking, or while listening to running water. Urge incontinence goes by other names as well: spastic bladder, overactive bladder, or reflex incontinence. This type of incontinence, characterized by the need to urinate more than seven times a day or more than twice each night, is the most common type of incontinence in elderly people.
Overflow incontinence is characterized by frequent or constant dribbling urine. Those with overflow incontinence are unable to completely empty the bladder, which fills up and then overflows, causing leakage. Sufferers of overflow incontinence often have the sensation of never fully emptying their bladder, and when they urinate, they produce only a weak stream of urine. This type of incontinence is common with people who have damaged bladders or blocked urethras. It can also be a result of nerve damage from diabetes.
To summarize, the symptoms of incontinence include urine leaks during a sneeze, laugh, or cough; urine leaks when lifting or running; not enough time to reach a toilet once the urge to urinate is felt; urine continuing to dribble after urinating; urine leakage following an intense desire to empty the bladder; and continual leakage of urine.
Continue reading to learn the common causes of incontinence during menopause to better know how to treat it.
Causes of Incontinence
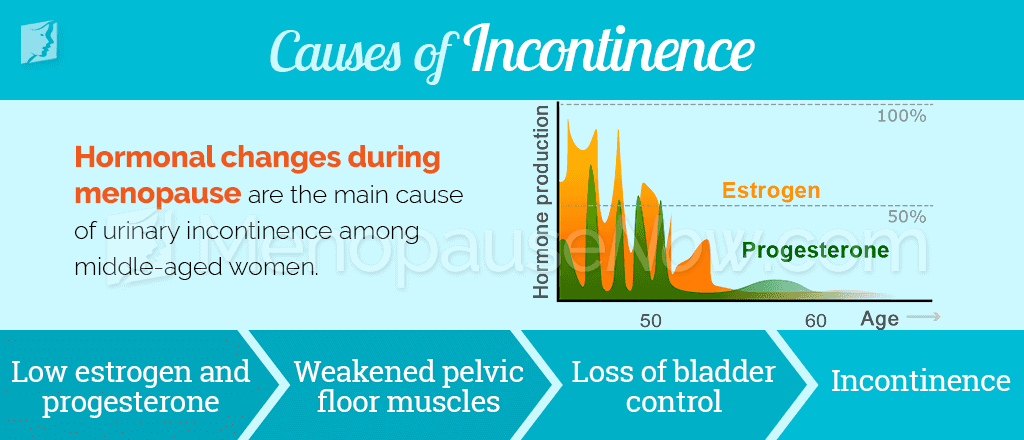
Because stress incontinence is the most common type of incontinence in menopausal and postmenopausal women, it's appropriate to begin there. This type of incontinence in women is almost always caused by hormonal imbalance, specifically decreased estrogen levels.
Estrogen helps to keep a woman's muscles strong, even the muscles that enable her to maintain bladder control. Estrogen also contributes to the health of the urinary tract lining. When estrogen levels begin to drop, as they do during menopause, the muscles weaken, and bladder control becomes increasingly difficult.
Other causes of incontinence
Although decreased estrogen levels primarily cause incontinence in menopausal women, there are additional causes of incontinence, but they tend to be more closely aligned with urge or overflow incontinence.Continue reading to learn more about the treatment options available for incontinence.
Incontinence Treatments
Fortunately for women who suffer from incontinence, there are several treatment options to make this menopause symptom a thing of the past. It's best to begin with the least obtrusive treatment, lifestyle changes, then move onto additional measures - like alternative medicines and finally medications or surgery - if incontinence persists.

A good way for a menopausal woman to alleviate incontinence is to strengthen her pelvic floor muscles, which support the bladder. There are several exercise techniques to accomplish this. To begin, lie on the floor and squeeze or pull in the pelvic muscles. Keep them tight for a count of three; release; rest for a few seconds; repeat. Decreasing caffeine and tobacco consumption is also recommended. These substances worsen incontinence.
The best way to combat incontinence is to combine lifestyle changes and alternative medicines. While a woman works to strengthen her pelvic floor muscles, she can also take certain herbs that help to stimulate natural hormone production, particularly estrogen.
For more prolonged or drastic cases of incontinence, it may be necessary to consult a healthcare professional and possibly seek surgical or pharmaceutical options, although these carry the most risk of side effects or complications.
It is generally recommended that women who suffer from incontinence and wish to treat it begin with lifestyle changes, then move onto alternative medicines, and finally, look to medications or surgery if nothing else seems to work. Click on the following link to learn specific treatments for incontinence in these three categories.
Sources
- National Institutes of Health. (2015). Kegel exercises - self-care. Retrieved May 13, 2016, from https://www.nlm.nih.gov/medlineplus/ency/patientinstructions/000141.htm
- National Institutes of Health. (2015). Stress urinary incontinence. Retrieved May 13, 2016, from https://www.nlm.nih.gov/medlineplus/ency/article/000891.htm
- Office on Women's Health. (2012). Urinary incontinence fact sheet. Retrieved May 13, 2016, from http://www.womenshealth.gov/publications/our-publications/fact-sheet/urinary-incontinence.html
- Quinn, S.D. & Domoney, C. (2009). The effects of hormones on urinary incontinence in postmenopausal women. Climacteric, 12(2), 106-113. doi: 10.1080/13697130802630083