Headaches during menopause can incapacitate women who experience them. For instance, in the case of migraine headaches, the pain generally comes on slowly on one side of the head, builds, and begins to pulsate and throb, often becoming severe enough to make exposure to light and noise too painful to endure. Chronic, severe headaches can negatively impact a woman's life in a number of ways. Fortunately, by better understanding headaches, women can find the best treatment options available based on their individual needs.
Continue reading below to learn all about headaches, as well as the types, causes, and treatment options.
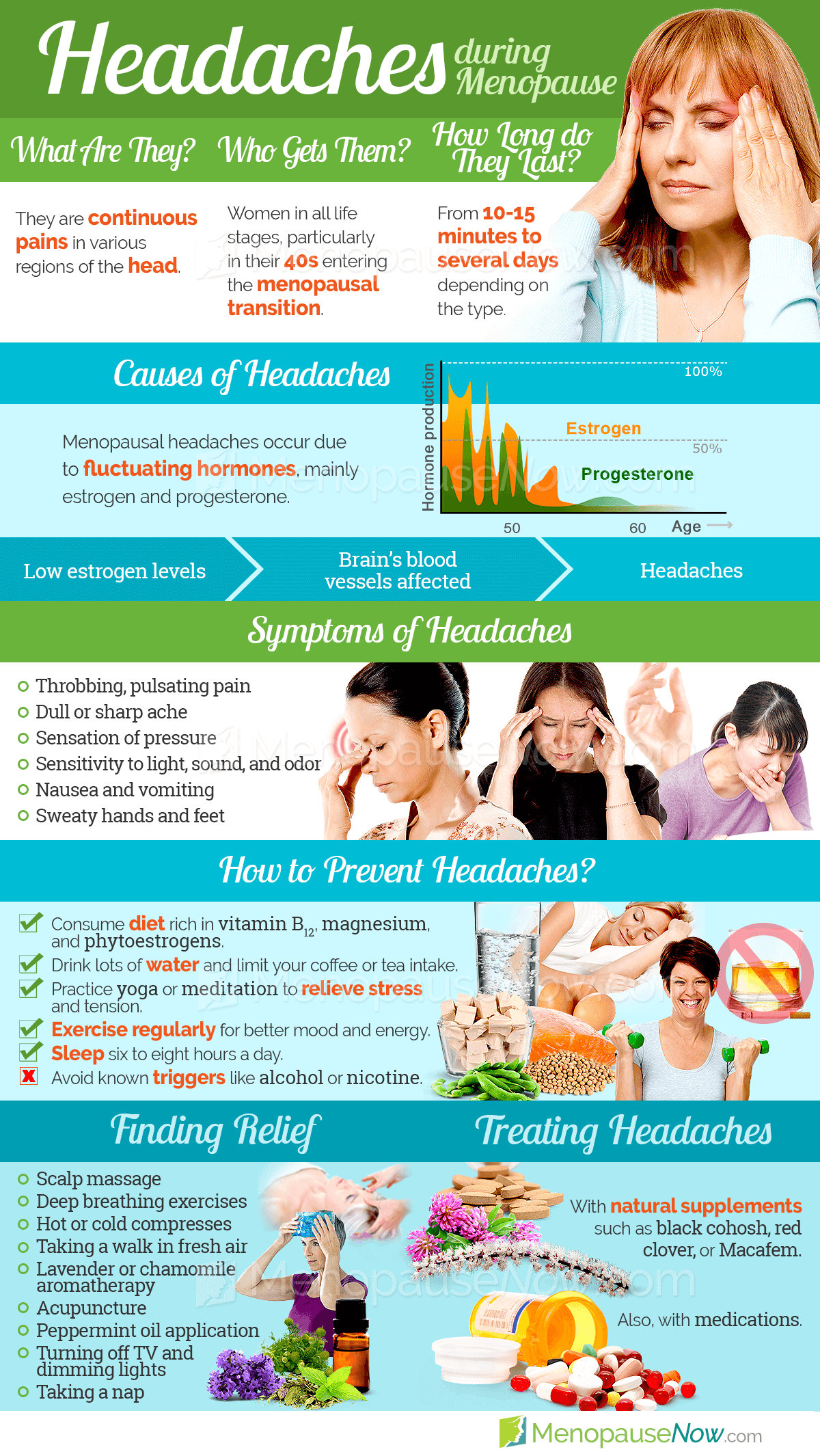
About Headaches
Women may experience headaches in many forms. Generally speaking, a migraine headache is a recurrent, throbbing headache generally felt on one side of the head but it may occur on both sides. It can last anywhere from one or two hours up to three days.
Many women entering perimenopause - the two to ten year period leading up to menopause - begin to experience more headaches than previously. There are several types of headaches that menopausal women may experience as a result of fluctuating hormone levels.
Common Symptoms of Headaches

- Throbbing, pulsating pain in the head
- Pain intensifies with routine physical activity
- Sensitivity to light, sound, and odor
- Nausea and vomiting
- Sweaty hands and feet
- Pain begins in a specific area on one side of the head
Click on the following link to learn more about headaches during menopause, or continue reading below to find out about the different types of headaches.
Types of Headaches
Some women might be familiar with menstrual migraines. Hormone-related, these migraines begin on the first day or two of menstruation and subside once menstruation finishes. Other types of migraines include the following:
Migraines with aura
These start with a neurological phenomenon (aura) experienced about half an hour before head pain arrives. Most auras are experienced visually, characterized by bright, shimmering lights around objects or at the edges of the field of vision.
Migraines without aura
This is the most common type of migraine. It can occur on one side or both sides of the head. Fatigue or mood swings may occur 24 hours before the headache. Nausea, vomiting, and sensitivity to light often accompany migraines without aura.
Other less common headaches include carotidynia, headache-free migraines, and ophthalmoplegic migraine.
Tension headaches are the most common type of headache, affecting 64% of men and 88% of women at some time during their life. A tension headache generally produces diffuse, usually mild to moderate pain throughout the head. The feeling has been likened to that of having a tight band cinched around the head. A tension headache may also cause pain in the back of the neck at the base of the skull.
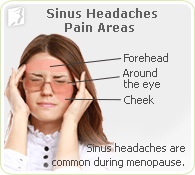
The third most frequently experienced type of headache in menopausal women is sinus headaches. Sinuses are air-filled cavities located in the cheekbones, forehead, and behind the bridge of the nose. The sinuses produce thin mucus that drains out of the channels of the nose. When a sinus becomes inflamed, usually as the result of an allergic reaction or an infection, the inflammation will prevent the outflow of mucus and cause a pain similar to that of a headache.
A sinus headache, then, is the inflammation and blockage of the sinus cavities. This is also known as congestion or a congestion headache.
In many cases, these three types of headaches can all be traced to the same cause. To learn more about these hormonal causes as well as other potential causes of headaches, keep reading below.
Causes of Headaches
Any woman who has found herself incapacitated with headache pain every time her period occurs has probably already made the connection between headaches and hormones, which wax and wane during menstruation. Similarly, hormonal fluctuations can spark painful migraine headaches.
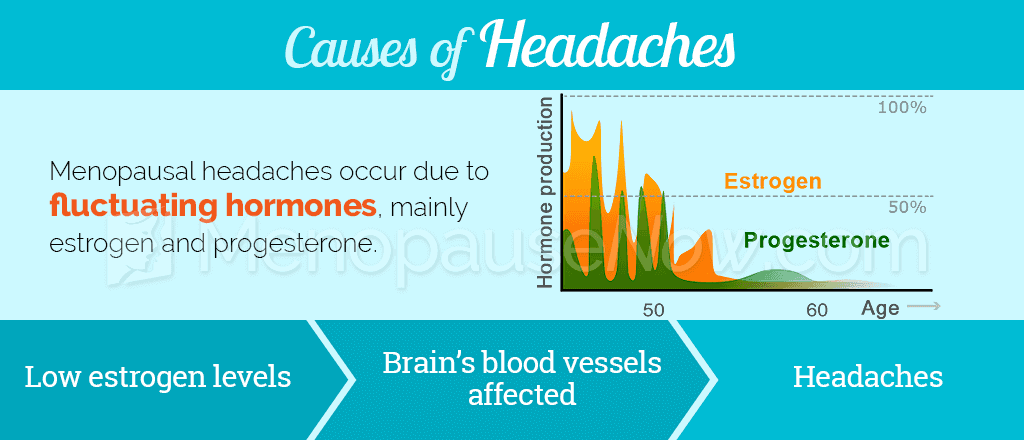
As menopause approaches, women's estrogen and progesterone levels surge and dip prior to the levels receding to a low level once she passes through menopause and no longer menstruates. This estrogen imbalance is known to affect the brain in various ways, including the onset of headaches.
Types of hormone-related headaches
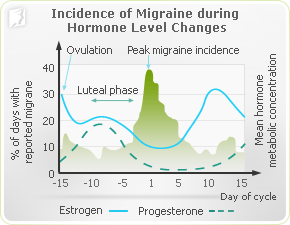
There are two main triggers for hormone-related headaches: headaches can be caused by declining estrogen levels or elevated estrogen levels. Dramatically-fluctuating estrogen levels just before menopause can cause both types of headaches. Many doctors believe that a long duration of significantly increased levels of estrogen, followed by a sudden drop in hormones, such as the time just before menopause, will cause more severe headaches than even menstrual headaches.
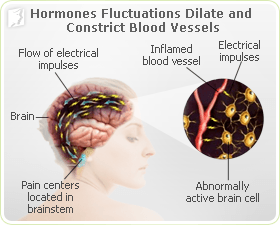
While the reason hormonal fluctuations cause headaches during menopause is still inconclusive, most researchers agree it has to do with the effects that hormones, such as estrogen and progesterone, have on the brain and its blood vessels. Estrogen causes blood vessels to dilate, while progesterone causes them to constrict. As the hormones fluctuate, the blood vessels are forced to expand and contract, resulting in intense pain in the head. Read below for additional causes of headaches during menopause.
Other causes and triggers of headaches
Although hormonal imbalance is the primary cause of headaches for women going through menopause, there are other factors that can either trigger or exacerbate headaches. The following triggers can set off headaches:
When to See a Doctor
The following symptoms warrant a trip to the doctor:
- Occurrence of a new, "worst-ever" headache
- Progressively worsening headaches
- More severe headache pain than usual
- Headaches that causes awakening from sleep
- Headaches and stiff neck along with a high fever
- Confusion, dizziness, or weakness with headaches
- Bright lights, loud noises, or strong odors
- Stress, anxiety, or relaxation after stress
- Weather changes
- Alcohol, caffeine (too much or withdrawal)
- Lack of or too much sleep
- Skipped meals or fasting
Foods that contain:
- Nitrates (hot dogs and lunch meats)
- Monosodium glutamate, better known as MSG (fast food, Chinese food, Parmesan cheese)
- Tyramine (aged cheese, soy products, fava beans, hard sausages, smoked fish, and Chianti wine)
Click on the following link to learn more about the causes of headaches, or continue reading below for a look at the treatment options available to alleviate headaches.
Headaches Treatments
Fortunately, there several treatment options for managing headaches. While many women turn to over-the-counter options such as aspirin for pain relief, this does not treat the hormonal imbalances that trigger them.

It is generally recommended that women begin with the least invasive option, which would be lifestyle changes. In the case of headaches, this involves avoiding environmental or dietary triggers, reducing stress with techniques such as yoga or meditation, and exercising. If headaches strike, management techniques such as massage or hot and cold compresses can help.
While these lifestyle changes are a good way to start managing headaches, the best option is usually to combine these changes with a more specific and direct approach.
Caffeine and Headaches
A cup of coffee or tea a day has been shown to reduce the incidence of headaches in menopausal women, though more than this may trigger headaches.Because headaches in menopausal women are typically caused by hormone imbalances, the most effective treatment method is targeting them at the source. A variety of natural and alternative medicines exist that are able to address this imbalance.
For more prolonged or drastic cases of headaches, it may be necessary to seek the advice of a healthcare professional and possibly seek pharmaceutical options, though these carry the most risk of side effects and are generally not recommended for long-term use in the treatment of headaches.
Click on the following link to learn more specifics about the treatments for headaches. The most effective treatments for headaches typically combine lifestyle changes and alternative medicine.
Sources
- MacGregor, E.A. (2009). Migraine headache in perimenopausal and menopausal women. Current Pain and Headache Reports, 13(5), 399-403. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/19728968
- National Institutes of Health. (2014). Headache. Retrieved April 21, 2016, from https://www.nlm.nih.gov/medlineplus/ency/article/003024.htm
- Office on Women's Health. (2012). Migraine fact sheet. Retrieved April 21, 2016, from http://womenshealth.gov/publications/our-publications/fact-sheet/migraine.html
- Ripa, P. et al. (2015). Migraine in menopausal women: a systematic review. International Journal of Women's Health, 7, 773-782. doi: 10.2147/IJWH.S70073